The theory of sugar addiction (or food addiction more broadly) is controversial. Despite what mainstream media or mosts health gurus have led you to believe, the research to date is inconclusive. As such, the current sugar detox frenzy is more misinformed fear mongering rather than anything actually substantiated by statistically significant, legitimate, long-term, peer-reviewed research.
I think it’s important to first acknowledge that you don’t need sugar, per se, for your physical wellbeing. You do need carbohydrates though and it’s very common for those concerned about eating sugar to throw a blanket over all types of carbohydrates and find themselves in restrictive eating patterns that aren’t nutritionally adequate. As such, I’m not so concerned with any argument over wether sugar is healthy or not, but what effect eliminating sugar (and any other carbs) has on food behaviors.
As I was digging into the research for this blogpost, it became overwhelmingly apparent that the rationale for researching food addiction or being concerned with possible addictive behaviors to food is deeply rooted in fighting the “obesity epidemic”. While I recognize that food behaviors are influenced by both genetics and environment, this is extremely concerning and exposes the first flaw in how we address this potential issue.
The reality is that weight stigma – or stereotyping based on a person’s weight – is positively correlated with body dissatisfaction and disordered eating. Conventional thought is that body discontent motivates someone toward healthy behaviors. Mounting evidence and clinical practice finds the opposite – body discontent is associated with disordered eating patterns, binge eating, lower levels of physical activity and increased weight gain over time.
One common stereotype and assumption made about those living in larger bodies is that they eat more. The individuals themselves can even internalize that belief and blame themselves for eating amounts that are actually adequate and no different than those in thin bodies. However, studies conducted on free living adults at a variety of BMI’s show little difference, on average, in calorie consumption. There is considerable difference for calorie intake within each BMI group, with many smaller people eating more than larger people. (Thanks to Fiona Willer for bringing this to our attention!) It’s important to challenge this assumption, since I do believe it fuels the idea that calorie restriction is necessary or even healthy for those classified as “overweight” or “obese”.
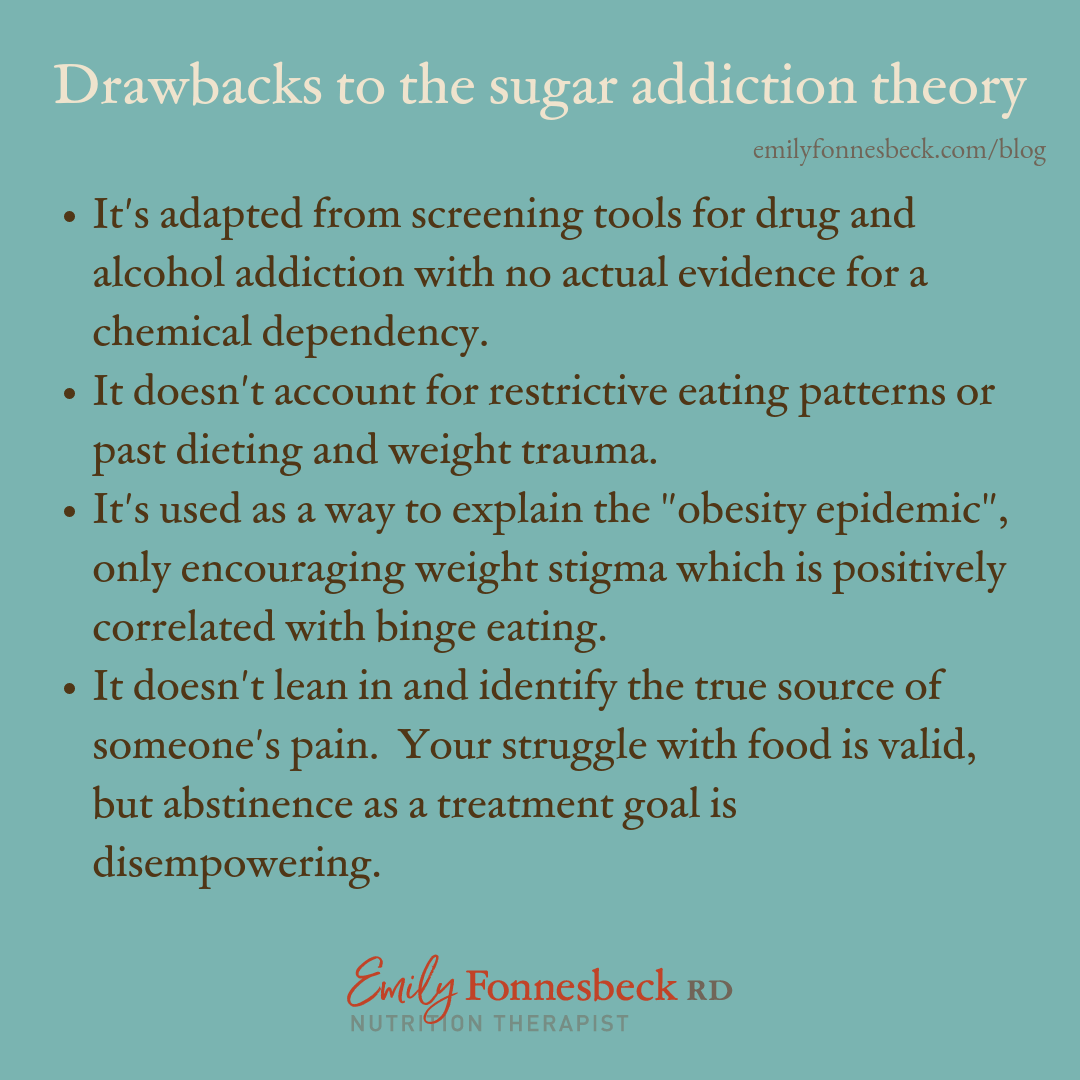
Further, the food addiction model has two specific drawbacks: 1) it was adapted from screening tools for drug and alcohol addiction 2) it doesn’t account for restrained or restrictive eating patterns. Clearly, these are huge read flags.
First, we can encourage abstinence from drugs and alcohol but not from food. You still need to eat, and I’d ask you this question: does declaring yourself an addict actually feel empowering? I suppose the idea of never eating sugar again and always saying no could make you feel “in control” but in my experience the opposite is true. Most people feel controlled by the food rules they’ve adopted and extreme shame if and when they disobey those rules.
You may have heard reports of studies on rats and how sugar lit up the same neural pathways as cocaine. Upon further inspection into those studies, this only occurred when rats underwent forced restriction…like a human on a diet. Deprivation increases the reward response from food, but doesn’t make the brain dependent on it. Also, those same reward centers respond when you listen to music, pet your cat or hear a baby giggle. And, you’re not a rat, so we need human studies to be able to fully apply any findings.
I heard this definition of addiction awhile back and I feel like it could apply here: “ Addiction is the result of unmet needs”. While I understand and recognize the chemical dependance on addictive substances like drugs and alcohol, that isn’t something we’ve found to be true with food. In addition, there may be the case for an “addictive brain”, and individuals predisposed to addiction could find they act impulsively around food, or substitute it’s use when abstaining from other substances. However, there’s a difference between using food as a way to consistently numb uncomfortable emotions and a legitimate addiction to food. In this way, avoidance may be the common denominator between drugs, alcohol and food, not addiction itself.
Proper treatment depends on proper diagnosis, and as far as the research is concerned, it’s likely more helpful to encourage alternative coping strategies for uncomfortable emotions or difficult life stressors than abstinence from sugar. From Linda Bacon, author of Health At Every Size: “Food is a wonderful source of pleasure, but it will get you into trouble if it’s the only source of pleasure you have in your life.”
Second, a sure fire way to make yourself preoccupied and obsessed with food is to restrict it’s consumption. Alternately, food habituation studies show us the more often you see a food, the less of it you eat (particularly when using mindful eating practices). Meanwhile, the food addiction scale assesses individuals based on their self-reported experiences with food. For example, some the questions read as follows:
- “I have found that I have elevated desires for or urges to consume certain foods when I cut down or stop eating them.”
- “My behavior with respect to food and eating causes significant distress.”
- “There have been times when I avoided professional or social situations where certain foods were available, because I was afraid I would overeat.”
These statements, and others on the scale, could apply to someone with an eating disorder or someone with a history of dieting and food restriction. What they may actually be assessing is disordered eating behaviors because of restricted and restrained eating patterns. In fact, just recently a client commented that she felt like she was probably addicted to sugar because she always wanted something sweet after a meal or couldn’t go even 3 or 4 days without wanting dessert. Well, me neither!! I worry that we are pathologizing very normal appetites for food when throwing around the idea of “sugar addiction” so carelessly.
My assessment is that the root issue isn’t a lack of ability to self-moderate sugar, but rather internalized weight bias. We are ENCOURAGING compulsive behaviors like binge eating by making weight the issue. Returning to my earlier point about weight stigma, fat phobia and the concern for “obesity” has led us to label individuals as addicts vs actually leaning in to identify the true source of someone’s pain. Compulsive behaviors are likely not symptoms of addiction but symptoms of distrust for your body, the fear of fat and a brain stuck in the diet mentality.
Alternately, a weight-inclusive approach is the belief that when given access to nonstigmatizing health care, we can maintain a healthy body and achieve a state of well-being regardless of size.
What I want to make certain is that I validate what may FEEL like food addiction. There are those of you reading who feel deeply troubled by your food behaviors and completely overwhelmed with how to heal. You need support, and I encourage you to seek professional help. While never eating sugar again may feel like the easiest and most logical solution, you can make peace with food without restriction. That process can be strategic, can include boundaries and can take your vulnerabilities into account. Please know that if food intake feels out of balance, you can learn how to self-moderate without swinging to the opposite extreme. That approach will include embracing your natural body size, using curiosity with food over judgment about food, and ensuring nourishing, adequate food patterns for a well-fed brain and body (regardless of it’s size).
Lastly, an all or nothing mentality is never helpful. Labeling sugar as “unhealthy” or “toxic” or “addictive” can easily lead to extremes in eating, which is more unhealthy than any one food. In fact, healthy behaviors and nutritious food patterns live in the grey. Balance, variety and flexibility is key to adequate nutrition. Ultimately, full permission to eat puts YOU in charge of YOUR food choices.
If you want further reading on this topic of food addiction, here are some other great resources:
Food Addiction: A Roundup Of Resources via Josee Sovinsky, RD
Can You Be Addicted To Food? via Vincci Tsui, RD
Sugar Addiction: A Summary Of The Science via Marci Evans, RD
Is Sugar Actually Addicting and Inflammatory via Robyn Nohling, RD
And definitely don’t miss this Nutrition Redefined Podcast episode with Stephanie and I where we talk a whole lot more about sugar addiction: You Don’t Have To Quit Sugar.
With confidence, Emily

Trackbacks/Pingbacks